HeLTI South Africa – BUKHALI Project
BUKHALI: BUilding Knowledge and a foundation for HeALthy lIfe trajectories
Bukhali is a Zulu word meaning smart/powerful, signifying the great potential benefit of optimizing women’s health for herself and her future offspring.
BACKGROUND
The health, societal and economic burden of non-communicable diseases (NCDs) is significant, increasing, and propagated by early life environments (undernutrition/stress) and later life adiposity, decreasing physical activity, increasing sedentary behaviour, poor dietary diversity, and intergenerational factors. The NCD burden falls heavily on low- and middle-income countries and this pattern is predicted to intensify dramatically in the near future. South Africa’s (SA) evolving burden of disease is complex due to:
- persisting malnutrition (infant stunting is 20%)
- high prevalence of overweight and obesity (OWO), particularly among women
- roughly 10-20% of school-age children are overweight or obese
- rising rates of NCDs such as type 2 diabetes (T2D) and mental health disorders
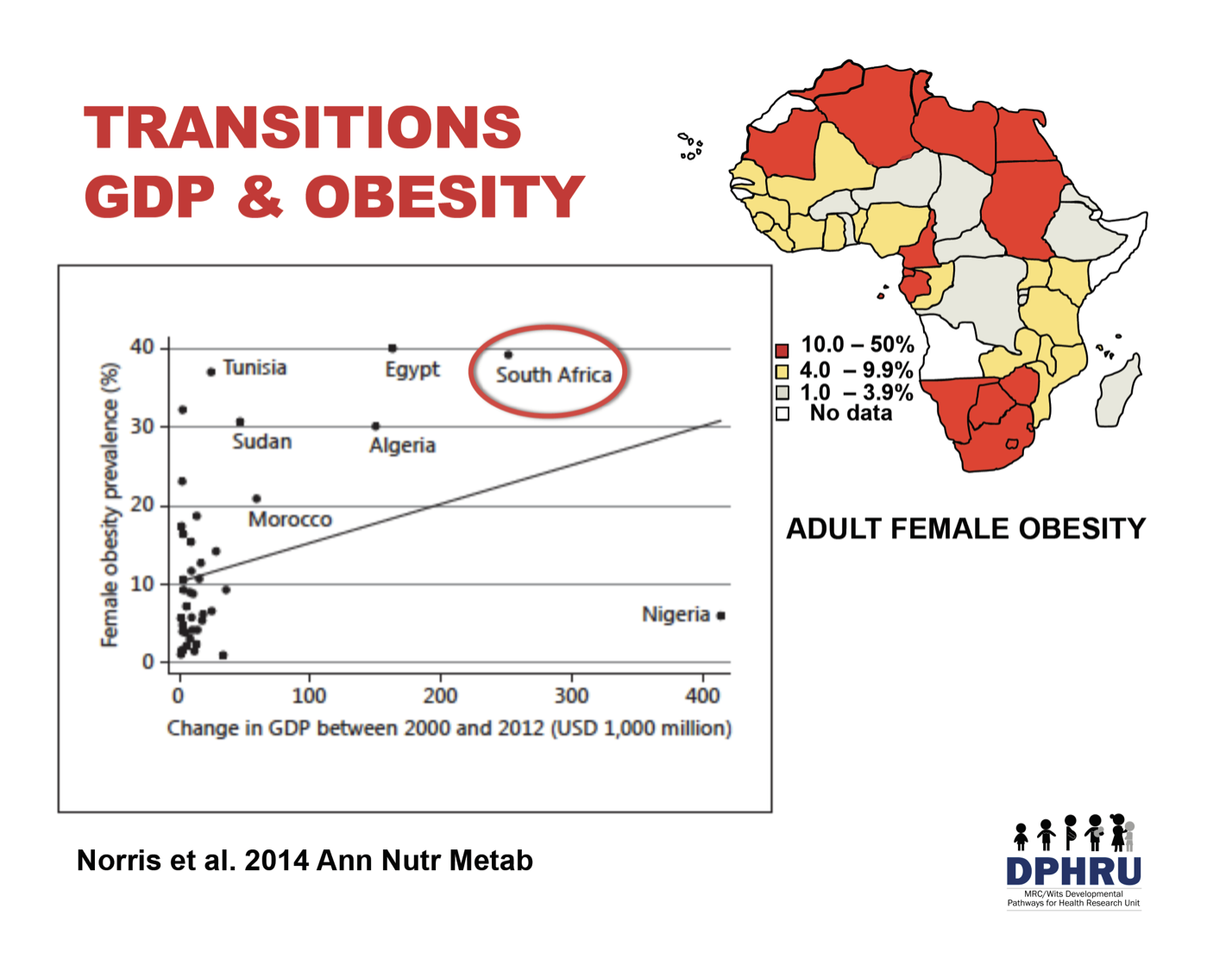
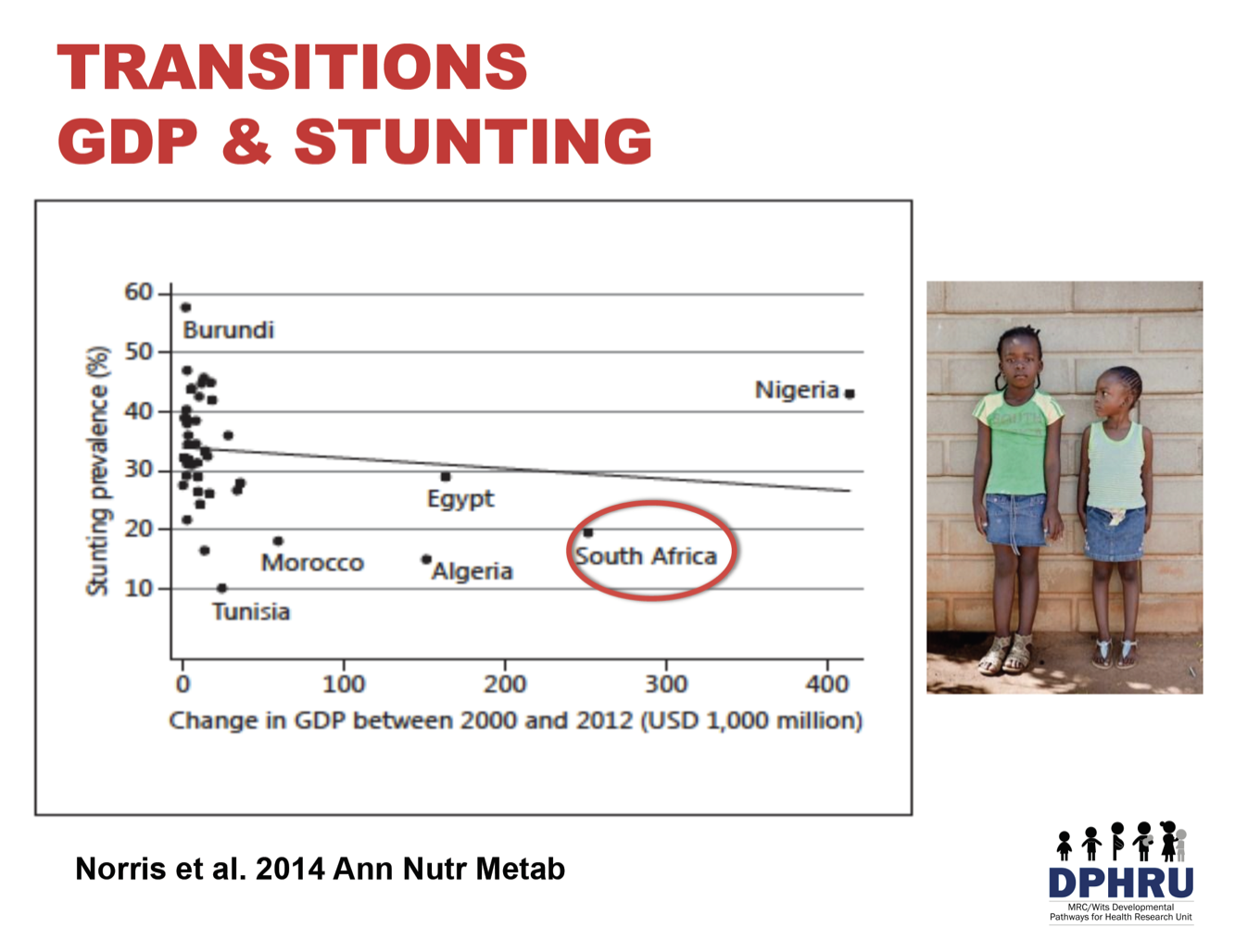
While the prevalence of child stunting tends to be inversely associated with economic growth, in several African countries the prevalence of adult female obesity shows the opposite association and closely mirrors their respective economic growth, with South Africa standing out. The two relationships are shown below. As African countries transition, adult obesity increases and child stunting decreases but still remains notably high, thus creating a scenario of a double burden of malnutrition in many African countries.
Obesity is increasing in Africa, particularly in women, and more specifically women residing in urban areas. South Africa has the third highest obesity prevalence in Africa (39.2%). In all countries in Africa, the obesity prevalence for females is significantly higher than that for males, with some countries reporting a 6- to 7-fold greater obesity prevalence between the two groups.
High levels of maternal obesity have serious consequences for both maternal and child health. For example, it has been linked to adverse pregnancy outcomes, such as hypertension, preeclampsia, gestational diabetes and delivery complications (Basu et al., 2010; Galtier-Dereure et al., 2000) as well as maternal morbidity and infant mortality (Black et al., 2013). However, many women enter their pregnancy overweight or obese and interventions aimed at maternal health may be too late to change the health trajectory of the mother and baby. Therefore, there is a need to begin laying the foundation for healthy trajectories by optimizing women’s health prior to and during pregnancy and reinforcing optimal health in the infant to offset obesity and NCD risk and improve cognitive development.
HeLTI – South Africa Study
To address the rising epidemic of NCDs, the Healthy Life Trajectories Initiative (HeLTI) was launched as a joint initiative between the Canadian Institutes of Health Research and the South African Medical Research Council. A local cohort study was established with the objective of measuring the long term impact of interventions delivered pre-conceptionally through early childhood on the improvement of maternal and child health, child development, and the prevention of NCDs.
A multi-faceted integrated intervention programme starting pre-conceptionally and continuing
The BUKHALI project has assembled a multidisciplinary team of experts from 7 institutions across South Africa and 6 institutions across Canada who are focusing on a longitudinal analysis of how early-life exposures in the preconception period and during pregnancy, infancy and childhood impact life-long trajectories of health and development of children in South Africa. Recruitment is currently underway.
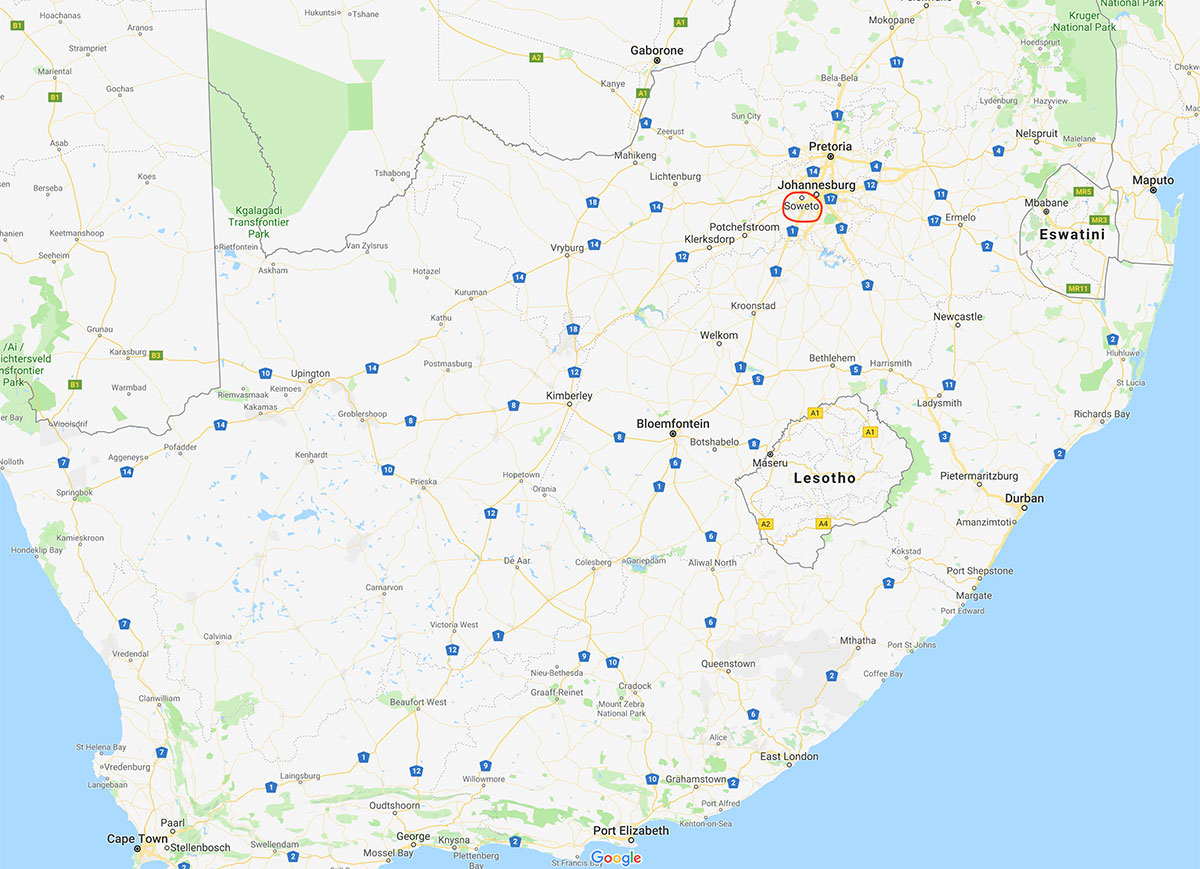
The study population is from Soweto, SA, where the SA team members have significant existing research infrastructure and demonstrated experience in recruitment for pregnancy and child cohort studies. By starting the integrated intervention (described below) pre-conceptionally in women and at appropriate points across the lifecourse (pregnancy, infancy and childhood), the intention is that this will improve cardiovascular and metabolic health, reduce childhood adiposity and improve child development outcomes. The aim is to ultimately reduce the risk of NCDs.
Using an individually-randomized design, the team is testing the efficacy of interventions that address behavior change to improve diet and physical activity during preconception, health during pregnancy, reduce perinatal depression, increase exclusive breastfeeding and improve parental nurturing care.
Aside from a one-month hard lockdown during the COVID-19 pandemic, the trial was able to resume operation mainly to maintain the trial participants on their respective regimens, incorporate COVID-19 support and surveillance protocols with a dedicated COVID-19 nurse, and engage with community households. After South Africa shifted to a level 1 stage (full economic activity with minimal restrictions), a revised community drive was launched to increase recruitment, which included pop-up stands, community forums, local newspaper advertisements, etc.
Intervention
Community health workers (CHWs) were trained in ‘Healthy Conversation Skills,’ a technique specifically developed and tested for use with socioeconomically disadvantaged participants to improve self-efficacy and support behavior change. CHWs will work in peer group sessions and have individual sessions with participants. The following four phases are broken down by their goals:
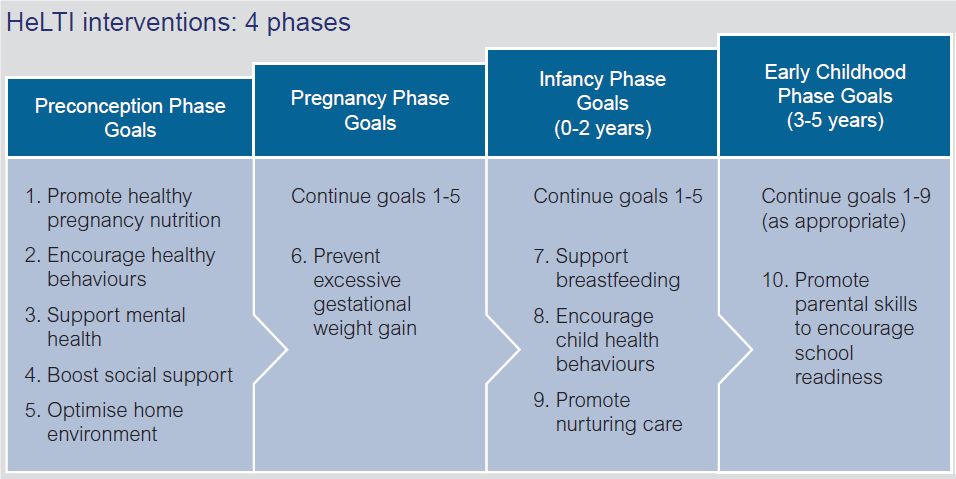
The primary outcome of the study is adiposity in children at age 5-6 years, measured by the Fat Mass Index. Other key outcomes include overweight and obesity and other indicators of body composition and distribution; glucose metabolism; blood pressure; and neurodevelopment. The project also includes a comprehensive series of measures to track maternal and child growth and development as well as the collection of biospecimens that will support studies into the science of the developmental origins of health and disease.
Find out more
Interested in learning more about Healthy Conversations Skills?
Mary Barker at the University of Southampton
Mary Barker and Wendy Lawrence’s presentation on HCS
Collaboration between the Universities of Southampton and Auckland: Click here
Or read an article assessing change in confidence and competence of staff working at Sure Start Children’s Centres using HCS.
Setting
Soweto (South Western Township) is a historically disadvantaged urban area of the city of Johannesburg covering 200 km2 (77.2 mi2). Over 1.3 million people reside in Soweto (6400/km2; 16,000/mi2) with 98.5% of the population Black South African. The University of the Witwatersrand is well known and respected within the community. The Wits Developmental Pathways to Health Research Unit (DPHRU) is where the study takes place. This is located within the Chris Hani Baragwanath Academic Hospital (CHBAH), a tertiary hospital in Soweto. Of adult women presenting at the CHBAH Antenatal clinic, 66% are either overweight or obese, 36% are anemic, 12% have gestational diabetes, and 31.2% are infected with HIV. Of the women who have delivered in the hospital, mean birthweight was 2.98 kg (SD 0.64) with 17.8% low birth weight and 3.5% macrosomic.
Previous studies have shown that the prevalence of overweight and obesity in women from this area increases from 10% by age 8 to 43% by age 22 years, while the prevalence in males remains fairly constant at 10%. If females are obese by age 5, they are 42.3 times at greater risk of being an obese adult.
Soweto represents a SA population at risk and where the planned intervention to reduce transgenerational risk of obesity and metabolic disease is needed and feasible.
Harmonization
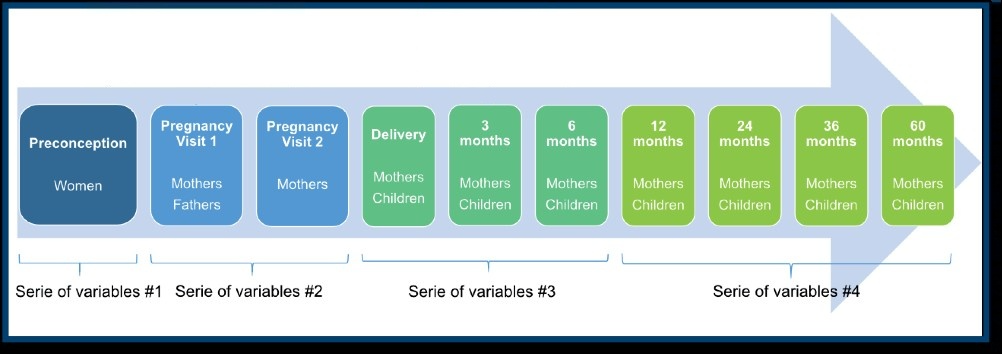
Senior members of the team are part of the HeLTI Harmonization Working Group. Their main goal is to harmonize core variable data collection across the four HeLTI country sites (Canada, China, India and South Africa). The figure below highlights the completed harmonized data collection within the preconceptual, pregnancy, delivery and infancy post-natal phases.
HeLTI-South Africa Team – South Africa
Tobias Chirwa, University of Witwatersrand
Lumbwe Chola, Human Science Research Council
Clive Gray, University of Cape Town
Heather Jaspan, University of Cape Town
Kathleen Kahn, University of Witwatersrand
Andre Kengne, South African Medical Research Council
Salome Kruger, North-West University
Vicki Lambert, University of Cape Town
Naomi Levitt, University of Cape Town
Lisa Micklesfield, University of Witwatersrand
Shane Norris, University of Witwatersrand (PI)
Thandi Puoane, University of the Western Cape
Michele Ramsay, University of Witwatersrand
Linda Richter, University of Witwatersrand
Marius Smuts, North-West University
Stephen Tollman, University of Witwatersrand
Mark Tomlinson, University of Stellenbosch
HeLTI-South Africa Team – Canada
Phillip Awadalla, Ontario Institute for Cancer Research
Diego Bassani, The Hospital for Sick Children
Zulfiqar Bhutta, The Hospital for Sick Children
Laurent Briollais, Sinai Health System
Bill Cameron, Ottawa Hospital Research Institute
Cindy-Lee Dennis, St. Michael’s Hospital
Barbara Fallon, University of Toronto
Jill Hamilton, The Hospital for Sick Children
Janet Jamieson, Red River College
Jennifer Jenkins, University of Toronto
Stephen Lye, Alliance for Human Development, Lunenfeld Tanenbaum Research Institute, Mount Sinai Health System (PI)
Stephen Matthews, University of Toronto
Daniel Roth, The Hospital for Sick Children
Stephen Scherer, The Hospital for Sick Children
Daniel Sellen, University of Toronto
Deborah Sloboda, McMaster University
Moshe Szyf, McGill University
Suzanne Tough, University of Calgary
Funded by: Canadian Institutes of Health Research and the South African Medical Research Council
For more information, please visit the HeLTI-South-Africa website.