Polyclinics
Delivering Comprehensive Community-Based Care
Community polyclinics and family doctors teams are the central piece of the most important health programs. The community polyclinic concept was introduced in 1976 and at the beginning they were responsible for providing primary health care. In 1984, the concept of the family doctor enhancing the health system’s ability to deliver on prevention and community-health analysis, as well as clinical services, was introduced. Since then, family physicians have worked with nurses, social workers, epidemiologists and psychologists as one team. Family physicians have specialized in pediatrics, obstetrics, gynecology, general medicine and epidemiology. Working in teams, they carry out health promotion, health education, and disease prevention activities, diagnose diseases, design health plans and community mobilization.
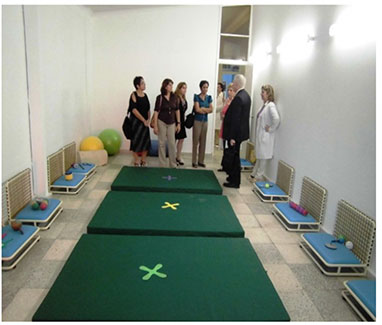
In January 2015 Drs. Stephen Lye and Yeneir Vera visited the Early Childhood Centre at the Polyclinic Julian Grimau in Arroyo Naranjo Municipality in Havana. The community based polyclinic houses many different medical offices and an Early Childhood Centre which has several stimulations rooms, incl. gym, visual stimulation, music, ballet, etc.
Primary Health Care – Role of the Polyclinics and Family Doctor Program
Cuba has a network of 473 polyclinics, each of which oversees thirty to forty family doctors. Family doctors, who live in and are part of the community, are responsible for the health of 150 to 200 families. The staff is multidisciplinary and includes a wide range of professionals. Currently, the average polyclinic offers 22 services, including rehabilitation, x-ray, ultrasound, optometry, endoscopy, thrombolysis, emergency services, traumatology, clinical laboratory, family planning, emergency dentistry, maternal–child care, immunization, and diabetic and elderly care. Various other specialties – including dermatology, psychiatry and cardiology – are available too, in addition to family and internal medicine, pediatrics, and obstetrics and gynecology.
The polyclinic is also a core for medical and educational training. Students in medicine and nursing receive part of their training at a polyclinic, which is often where they will work after graduation. Polyclinics collect data for important scientific research, and are conduits for scientific advances. The data collected are used by health authorities to evaluate the effectiveness of the polyclinic programs. Scientists are frequently appointed to polyclinics, where they undertake academic research and facilitate the transfer of knowledge to and from line staff.
Contribution of the Polyclinics to the Early Childhood Development System
Family Planning Consultations and Preconception Risk Program
Polyclinics have family planning consultations and preconception program. As part of this program, family doctors classify all women in childbearing age in their communities, according to potential risk factors for complications in pregnancy in the future, such as diabetes, high blood pressure, anemia, etc. Primary care staff work with women who wish to become pregnant to mitigate risk factors and plan conception for when the woman’s physical condition is optimal. The program is structured with specialized family planning consultations at all polyclinics which are equipped with effective and modern methods of fertility control and are aimed at cases of higher reproductive risk that cannot be solved with traditional methods or the family doctors. These consultations provide more specialized attention both in conception and infertility, and now provide prenatal care for patients with certain unresolved perinatal risk. The team includes gynecologists, family physicians, psychologists, social workers, nurse midwives and consultations with other specialists can be arranged. The objective of the program is to reduce the risk of pregnancy, the risk of low birth weight, the incidence of teenage pregnancy, the incidence of induced abortions and to ensure the quality of menstrual regulations and abortions if necessary. This program also facilitates increased participation of men in all family planning activities, provides appropriate services for infertility and at the same time participates in the established distribution of contraceptive methods and offers sterilization services for men and women.
National Maternal-Child Health Program (PAMI, the Spanish acronym)
The centralized Maternal-Child Health Program (Programa Nacional de Atencion Materno-infantil, or PAMI) was established in 1970. It has the main responsibility of ensuring the health of women of childbearing age. The success of PAMI’s efforts is documented by one of the most rapid declines in infant mortality ever recorded. Under the leadership of this program, governmental sectors as well as community organizations collaborate to provide prenatal care and other health services to women and their children. Such services include free screening and diagnostic testing as well as the availability of maternity homes in every municipality to provide medical assistance and nutritionally balanced, calorically dense meals 24 hours/day for women with high-risk pregnancies. According to World Bank data, 100% of pregnant Cuban women receive prenatal care, defined as medical and nursing care recommended for women before and during pregnancy.
Maternal visits and screening during pregnancy
Upon conception, pregnant women are seen once per month during the first 33 weeks of pregnancy. At the first visit following conception, the level of nutritional risk is determined using the mother’s initial body max index (BMI). Additional measures of pre- and postnatal care are provided in Table 1. If the pregnancy is categorized as high risk according to the Cuban Pregnancy Weight Gain Guidelines, women are seen at more frequent intervals or referred to a maternity home for the duration of their pregnancy. In addition, all pregnancies deemed high risk follow a “partogram” or critical care route outlined for all clinicians attending to these women. Under this innovative care plan, the care of each gravid will be transferred early in the pregnancy to the physicians and hospitals best-suited for delivering the newborns based on the individual conditions that place them at high risk. For all normal to moderate-risk pregnancies, visits occur twice monthly during weeks 34 through 38, after which time weekly visits are initiated. If the pregnant woman fails to show up to a clinic visit, the primary care physician visits the home for the required visit, this is unique to the Cuban model. Also of interest, primary care physicians within each municipality deliver infants unless complications arise that warrant an obstetrician. In keeping with the comprehensive approach to health care in Cuba, the newborn and its mother are seen weekly by their primary care physician through the first 3 months of life, after which time mother and child transition to monthly visits through the first year of life. Such comprehensive approaches to providing adequate primary care in Cuba have assisted the country in accomplishing an infant mortality rate lower than most other Latin American countries and the United States and similar to that of Canada.
Maternity Homes
The country has a network of 289 maternity homes for pregnant women exhibiting hypertension, anemia, malnutrition, excess weight, or other health complications or for those who simply live far from a maternity clinic. The purpose of maternity homes is to provide general care for pregnant women to prevent complications related to pregnancy. A typical maternity home has 20 nurses and 5 doctors, 2 obstetric/gynecological specialists and 1 doctor with specialization in nutrition. It has on-site dentistry, ultrasound and laboratory services, with 50 beds for inpatients.
National Genetics Program
All pregnant women and newborns are evaluated by the genetic risk assessment service located in every polyclinic. These genetics services are supported by municipal, provincial and national medical genetics centres that implement the National Program for Diagnosis, Management and Prevention of Genetics Diseases and Congenital defects.These genetics services are supported by 169 Municipal Centers of Medical Genetics, 14 Provincial Centers of Medical Genetics, and the National Centre of Medical Genetics, all of which are staffed by geneticists, genetic counselors, nurses and technicians (the total accounts for about 1 genetics counselor for 17,536 inhabitants). Together, these professionals and technicians implement the National Program for Diagnosis, Management and Prevention of Genetic Diseases and Congenital Defects.
Human Breast Milk banks and breastfeeding
Iron deficiency anemia is considered a national health priority, especially pregnant women, newborns, and children under five years old. Public health authorities had developed policies to reduce the prevalence of anemia. Multisectorial strategy included distribution of iron fortified food and supplements, beefed-up nutritional guidelines, education and greater iron deficiency survellaince. Also, Cuba started the implementation of the National Breastfeeding Program and human breast milk banks with the objective to increase the percentage of women breastfeeding exclusively for the first six months of their child’s life up to two years with supplemental food and reduce morbidity and mortality among very low birth weight babies.
Immunizations Campaigns
All of the staff at the polyclinic are familiar with and responsible for the community. They encourage immunization campaigns through house calls, home visits and semi-annual check-ups. This makes Cuba extremely effective in controlling everyday health issues. Having doctors’ offices in every neighborhood has brought Cuba an unmatched record in dealing with chronic and infectious diseases with amazing limited resources. These include (by date eradicated): polio (1962), malaria (1967), neonatal tetanus (1972), diphtheria (1979), congenital rubella syndrome (1989), post-mumps meningitis (1989), measles (1993), rubella (1995), and TB meningitis (1997).
Developmental Care Visits (Puericultura)
All newborns are seen the first seven days of life by the family doctor in the medical office or in their homes. With the first assessment, they can identify any problems related to the newborn or the mother. The nurse counsels the new mother about the correct technique for breast feeding, newborn nutrition, immunization, vitamin supplementation and also contraceptives methods that they can use during the first year. Also, the nurse takes the infant’s measurements (weight for age, length for age and head circumference. Some of the consultations are supervised by the pediatrician who is working with the team.
The family physician should know the risk categories of the children in their care, so that they can plan actions to reduce morbidity and mortality as well as to modify risk. Risk situations are considered: low birth weight, gestational age less than 37 weeks, multiple pregnancies, and nutritional risk, no breastfeeding in less than 6 months, previous admissions for various reasons (IRA-EDA), social risk (dysfunctional family, teenage mother), other conditions that the team considers basic health risk.
The most revolutionary idea of the Cuban system is doctors living in the neighborhoods they serve. A doctor-nurse team are part of the community and know their patients well because they live at (or near) the consultorio (doctor’s office) where they work. Consultorios are backed up by Polyclinics which provide services during off-hours and offer a wide variety of specialists. Polyclinics coordinate community health delivery and link nationally-designed health initiatives with their local implementation.
Maternal and Child Health Indicators
Early diagnosis, research, assessment, and ongoing monitoring are key elements of Cuban health programs. Effective screening procedures such as: early detection of high risk pregnancies, bi-annual medical check-ups, early recognition of childhood developmental problems, all enable intervention at an early stage and avoid more costly remedies later in life. While infant mortality under 5 per 1000 live births, and low birth weight newborns are just 5.4%. Cuban health authorities and professionals are less satisfied with progress in reducing maternal mortality. In 2010, the maternal mortality ratio was 43.1 (per 100,000 live births); 29.7 direct maternal mortality, and 13.3 indirect—well below the 85 registered in 2008 for Latin America and the Caribbean, but still considered unsatisfactory. This has led to a national review of protocols, facilities, human resources, and preventive approaches in order to achieve further reduction of maternal deaths. Women’s education about their own bodies, better identification by the health system of at-risk women, and concentration of high-tech resources where they are most needed are some of the responses already been implemented.
